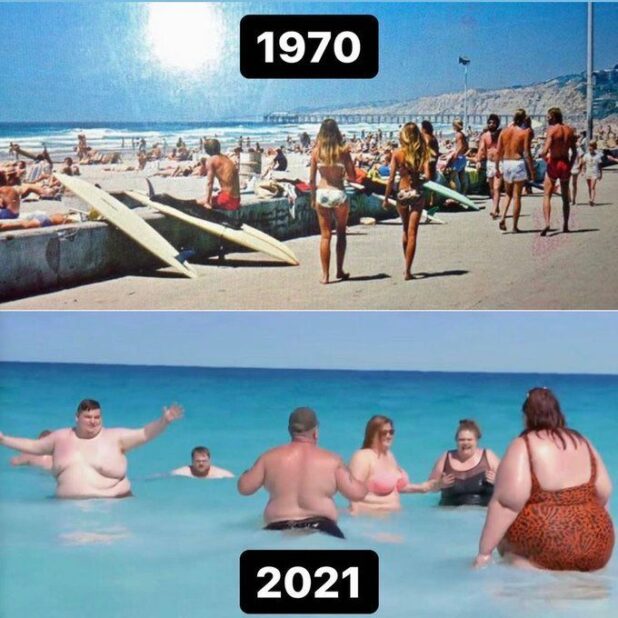
Wait, I thought being obese was healthy?
I’ve seen all of these advertisements…
AP:
Children struggling with obesity should be evaluated and treated early and aggressively, including with medications for kids as young as 12 and surgery for those as young as 13, according to new guidelines released Monday.
The longstanding practice of “watchful waiting,” or delaying treatment to see whether children and teens outgrow or overcome obesity on their own only worsens the problem that affects more than 14.4 million young people in the U.S. Left untreated, obesity can lead to lifelong health problems, including high blood pressure, diabetes and depression.
“Waiting doesn’t work,” said Dr. Ihuoma Eneli, co-author of the first guidance on childhood obesity in 15 years from the American Academy of Pediatrics. “What we see is a continuation of weight gain and the likelihood that they’ll have (obesity) in adulthood.”
For the first time, the group’s guidance sets ages at which kids and teens should be offered medical treatments such as drugs and surgery — in addition to intensive diet, exercise and other behavior and lifestyle interventions, said Eneli, director of the Center for Healthy Weight and Nutrition at Nationwide Children’s Hospital.
In general, doctors should offer adolescents 12 and older who have obesity access to appropriate drugs and teens 13 and older with severe obesity referrals for weight-loss surgery, though situations may vary.
The guidelines aim to reset the inaccurate view of obesity as “a personal problem, maybe a failure of the person’s diligence,” said Dr. Sandra Hassink, medical director for the AAP Institute for Healthy Childhood weight, and a co-author of the guidelines.
“This is not different than you have asthma and now we have an inhaler for you,” Hassink said.
Young people who have a body mass index that meets or exceeds the 95th percentile for kids of the same age and gender are considered obese. Kids who reach or exceed the 120th percentile are considered to have severe obesity. BMI is a measure of body size based on a calculation of height and weight.
Obesity affects nearly 20% of kids and teens in the U.S. and about 42% of adults, according to the Centers for Disease Control and Prevention.
The group’s guidance takes into consideration that obesity is a biological problem and that the condition is a complex, chronic disease, said Aaron Kelly, co-director of the Center for Pediatric Obesity Medicine at the University of Minnesota.
“Obesity is not a lifestyle problem. It is not a lifestyle disease,” he said. “It predominately emerges from biological factors.”
The guidelines come as new drug treatments for obesity in kids have emerged, including approval late last month of Wegovy, a weekly injection, for use in children ages 12 and older. Different doses of the drug, called semaglutide, are also used under different names to treat diabetes. A recent study published in the New England Journal of Medicine found that Wegovy, made by Novo Nordisk, helped teens reduce their BMI by about 16% on average, better than the results in adults.
If the government actually cared about obesity, they would regulate the food industry.
A “sedentary lifestyle” does not cause obesity. It is the food.