These people are trying to ban smoking, because they love you so very much and sit at home at night worrying about your health.
They love you so dearly that they want to stop you from using butter and instead force you to use the much healthier alternative, partially hydrogenated vegetable oil.
Their heart goes out to you to such an overwhelming degree that they will force-vaccinate you to save you from the flu.
Seatbelt laws.
But if you’re obese, that’s fine. It’s very healthy to be obese and in fact, people should get fatter and fatter for health reasons, say they.
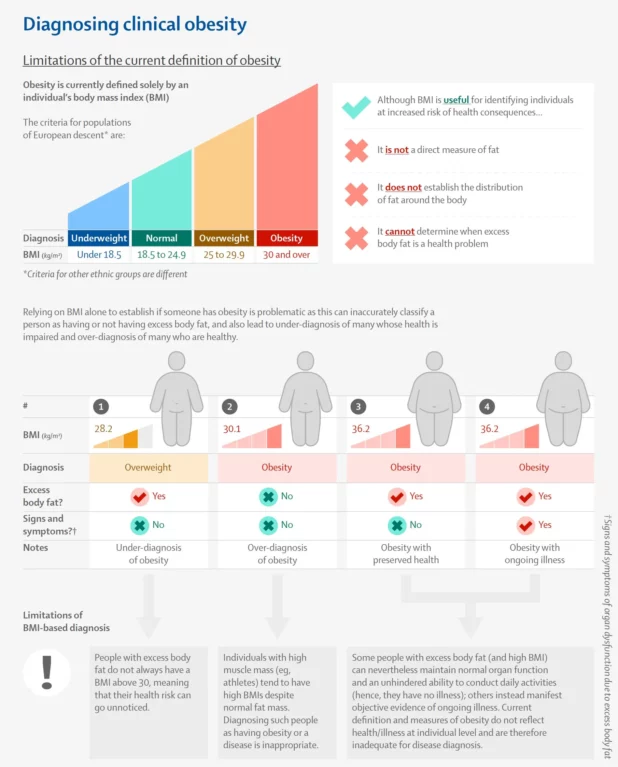
Doctors are proposing a “radical overhaul” of how obesity is diagnosed worldwide amid concerns that a reliance on body mass index may be causing millions of people to be misdiagnosed.
More than 1 billion people are thought to be living with the condition that for decades has been diagnosed by measuring a person’s BMI (their ratio of height to weight) to estimate the amount of excess body fat they have.
However, there are fears BMI on its own is not a “reliable measure” of an individual’s health and may be resulting in both under- and over-diagnosis of obesity, with “negative consequences” for those affected and wider society.
Dozens of the world’s leading experts across a broad range of medical specialisms – including endocrinology, internal medicine, surgery, biology, nutrition and public health – are now calling for a “reframing” of the condition that is causing major harm on every continent and costing countries billions.
Relying only on BMI is “ineffective” because it is not a direct measure of fat, fails to reflect fat distribution around the body, and does not provide information about a person’s health, according to a report published by the experts in the Lancet Diabetes and Endocrinology journal.
The proposed shake-up, endorsed by more than 75 medical organisations around the world, puts forward new ways to diagnose obesity based on other measures of excess body fat in addition to BMI, such as waist-to-hip ratio or waist-to-height ratio, as well as objective signs and symptoms of ill health.
At the moment, some people with excess body fat do not have a BMI that indicates they are living with obesity, meaning potentially serious health problems are going unnoticed and untreated. At the same time, others with a high BMI may be diagnosed with obesity despite maintaining normal organ and bodily functions, with no signs or symptoms of ongoing illness.
Prof Francesco Rubino, the chair of the Lancet commission which produced the report, said the changes would provide an opportunity for health systems globally to adopt a universal, clinically relevant definition of obesity and a more accurate method for its diagnosis.
He said: “The question of whether obesity is a disease is flawed because it presumes an implausible all-or-nothing scenario where obesity is either always a disease or never a disease. Evidence, however, shows a more nuanced reality. Some individuals with obesity can maintain normal organs’ function and overall health, even long term, whereas others display signs and symptoms of severe illness here and now.
BMI is frankly a fine measure. Sometimes the measurements can get complicated with top level fitness people, but that is only an issue of the way it is measured.
If you measure it correctly, using more expensive and advanced methods, it always works on any body type and will give you a clear image of the person’s overall fitness with relation to muscle-to-fat ratio.